Many runners present to our clinic complaining of tightness down the outside of their leg or pain over the outside of their knee. The common diagnosis is ITB friction syndrome, but what does this mean and how do you we treat it?
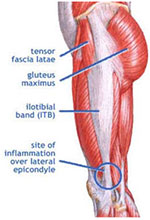
Firstly it is important to identify what the Illiotibial band (ITB) is and its purpose when running. The ITB is attached to the Tensor fascia late (TFL) muscle that attaches along the crest of the pelvis. It forms a long thick tendon which attaches to the Tibia below the knee (Gerty’s tubercle). The main role of the ITB is to support the weight bearing hip in single leg stance by creating an abduction moment (sideways force) at the hip joint. This force works with the gluteal muscles to stop the opposite hip from dropping while running. There are other actions that the TFL and ITB perform during running such as extending the hip and flexing the knee, but these are only secondary movements and are not directly related to the role of the ITB during running. As you can see in the picture below in (A) the Tensor fascia late muscle is contracting stopping the pelvis from dropping. If this muscle starts to fatigue as seen in (B), then the level of the non stance hip drops and the stance hip shifts out to the side placing greater tension on the ITB. This raises the question as to whether the ITB is tight or is there weakness and fatigue causing the ITB to be put under greater tension.
In my experience I feel the hip weakness to be more of an issue in runners, particularly extreme distance running where the running speed is somewhat slower but the repetitive strain is much greater.

Treatment
While the exact cause of the pain in ITB friction syndrome has not been exactly identified in the research to date, there is an acute phase to this injury where the pain needs to be controlled. This unfortunately means stopping of running for a period of time. I have tried to treat mild cases of the condition while athletes continue to run but it does not provide optimal results. How long an athlete requires off running mainly depends on how long they have been experiencing symptoms. I feel between 3-8 weeks is often required to settle most athletes symptoms.
The importance of finding a way to exercise during this period is crucial to the overall success of the rehabilitation period. This syndrome is driven by weakness and fatigue which we do not want to exacerbate by resting athletes. Therefore the use of a bike if able or swimming with a pool buoy may be required in the more extreme cases.
While the symptoms are settling the treating therapist aims to correct biomechanical deficiencies and possible training or technique errors in the athletes running. The most common treatment method is to massage the ITB or use a foam roller with the thought of lengthening/stretching the tendon. Given that tendons throughout the body are non-contractile tissue the effectiveness of lengthening/stretching the ITB is questionable. Patient’s at times report temporary relief of symptoms; however I see very little long term benefit from this treatment and it can lead to long term use of rollers for very little gain. Instead I feel it is important to identify the weakness in the athlete’s running technique and training methods that need addressing.
There are common weaknesses seen in athletes with ITB injury, however every patient is very different and these generalisations should only be used as a guide. When looking at the pelvis the muscle groups involved often include the TFL and Glut Medius as they directly control the position of the hip at ground contact and the degree of hip drop of the contralateral hip. Secondary to these muscle groups the Obliques and Quadratus Lumborum on the opposite side to the injured limb also eccentrically control the degree of hip drop also. These muscle groups work in an eccentric (lengthening), closed chain position while running. Therefore where able once the athlete’s pain has started to settle, time and repetition needs to be applied towards training these muscle groups in this specific manner. It is then very important that the athlete builds up there rehabilitation to the point where the duration and intensity of their rehabilitation is equivalent to their expected time and intensity of their running. Simply 3×10 is not going to cut it. Finally once the patient has returned to running a very gradual return is required and I often recommend a 3 week on: 1 week off running programme for the first 3 months to minimise the chance of repeating the overload that lead to the injury originally. In cases where there are repeated episodes an athlete’s running technique needs to be corrected.
I hope this provides some background information on the cause and management of ITB injuries and provided more options then simply rolling on a foam roller, happy running.

One thought to “Illotibial Band”
Pingback: Running injuries | Sydney CBD | Injury Prevention & treatment
Comments are closed.